Medicaid is a joint federal and state program that provides health insurance to low-income individuals and families. The program also covers medications for disables and certain elderly individuals. It is administered by each state and the specific benefits may vary slightly from state to state. Medicaid also covers a wide range of prescription medications including both generic and branded drugs. In this detailed guide, you may know everything about Medicaid covered prescriptions and Medicaid prescription drug coverage.
Remember! For the prescription drug coverage, Medicaid may require prior authorization or impose limits on certain prescription medications and people may need to be eligible for certain prescription programs. Many states like Maryland have already implemented many Medicaid-managed care programs and they are run by the help of private insurance companies to provide Medicaid benefits with prescription drug coverage.
Does Medicaid Cover All Prescriptions?
Medicaid generally covers a wide range of prescription medications to the eligible individuals; however, Medicaid may not cover all prescriptions for every individual. Medicaid coverage may be limited or excluded for certain types of medications or certain medical conditions. For example, Medicaid may not cover medications that are not medically necessary or that are experimental or investigational. Furthermore, Medicaid may have limits on getting a prescription refilled early each month or may need authorization for certain medications. It is always a good idea to check with your state Medicaid agency or your Medicaid managed care plan. In this way, you can verify what medications are covered under your specific plan.
Does Medicaid Cover Compounded Prescriptions?

Medicaid may cover compounded prescriptions for some people who are eligible for the program. Compounded prescriptions are medications that are prepared by a pharmacist by combining, mixing or altering ingredients to meet the specific needs of the patient. Compounded prescriptions may be used to create a medication in a form that is easier for a patient to take such as a liquid or a topical cream. You can also choose to customize a medication to meet your specific needs if you have an allergy or intolerance to certain ingredients. For this, you should know about pharmacy prescription rules and regulations.
Does Medicaid Cover 90-Day Prescriptions?
Yes, Medicaid generally covers 90-day prescriptions. In general, Medicaid allows the filling of prescriptions for a 90-day supply at a pharmacy. This can be more convenient for patients because it allows them transferring prescriptions between pharmacies. So, it can be the best choice for those who want to save money on medications.
Does Medicaid Cover Alternative Medicine?

Medicaid coverage for alternative medicine may vary depending on the specific state in which you reside and the specific alternative medicine treatment that is being sought. Some states may cover certain alternative medicine treatments such as acupuncture or chiropractic care. Medicaid coverage for alternative medicine treatments may be excluded in some cases. For example, Medicaid may not cover alternative medicine treatments that are experimental or that are not supported by scientific evidence.
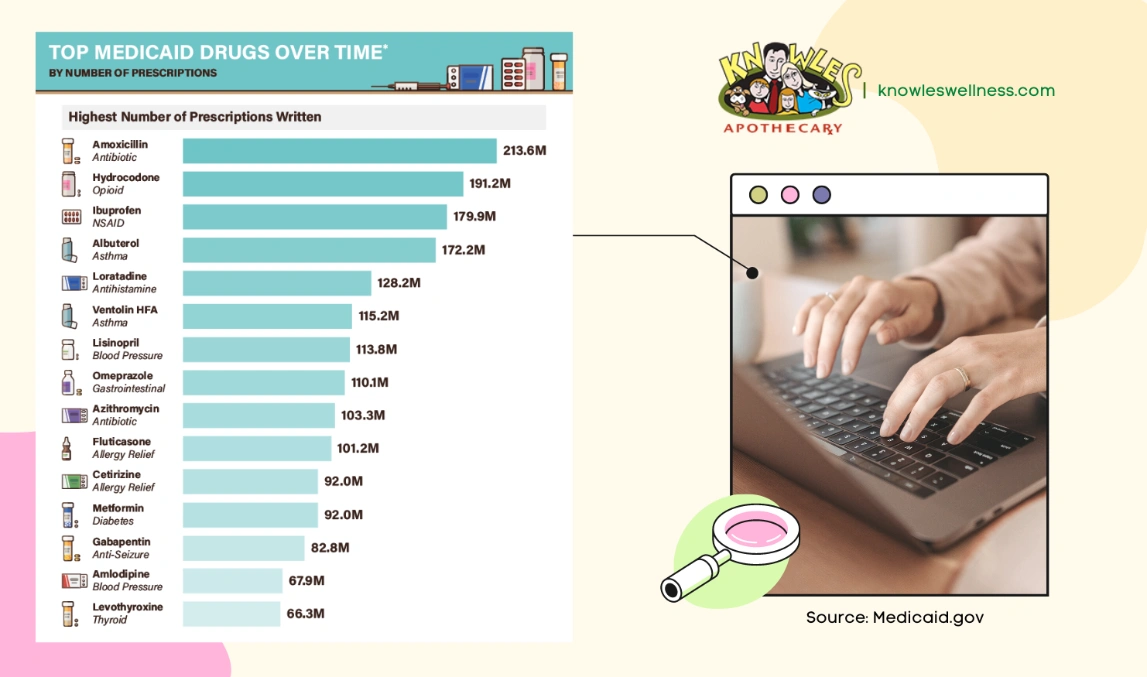
What Medications Does Medicaid Not Cover?
In general, Medicaid covers a wide range of prescription medications but it does not cover drugs for weight loss or weight gain. It also provides no support for non-prescription drugs. Thus, the coverage may be limited for various types of medications or medical conditions.
How Many Prescriptions Does Medicaid Cover per Month?
The number of prescriptions that Medicaid covers per month may vary depending on the specific state in which you reside and the specific medications. Medicaid may have limits on the number of prescriptions that an individual can fill each month. For example, Medicaid may limit the number of prescriptions filling a long time that an individual can fill each month to a certain number. Medicaid may also have limits on the number of refills that are allowed for certain medications. Furthermore, Medicaid may need authorization which means that the individual must need approval from Medicaid before filling the prescription.
Does Medicaid Cover Prescriptions in Maryland?
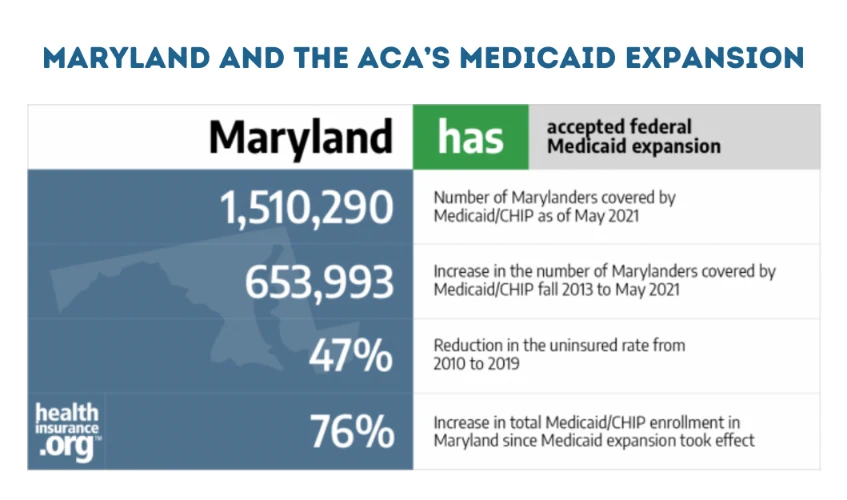
Medicaid generally covers prescription medications for individuals. In Maryland, Medicaid is administered by the Maryland Department of Health (MDH). The MDH operates several Medicaid programs, including the Maryland Medical Assistance Program (MMAP). It provides health coverage for low-income individuals and families. The MMAP covers a wide range of prescription medications for individuals who are eligible for the program. You can refill your prescription online in MD because Medicaid beneficiaries may be able to fill their prescriptions at a pharmacy or have their medications mailed to them through the MDH’s Mail Order Pharmacy program. Medicaid beneficiaries may also be able to fill their prescriptions at a participating retail pharmacy through the MDH’s Retail Pharmacy Program. To learn more about Maryland and the ACA’s Medicaid expansion, click here.
Takeaway
It is always a good idea to check your Medicaid-managed care plan to verify what medications are covered under your specific plan and to confirm any limits or requirements that may apply to your certain case because you should always follow the prescription laws in Maryland. You can also discuss your options with the doctor or pharmacist to determine the best course of treatment for your specific needs.


